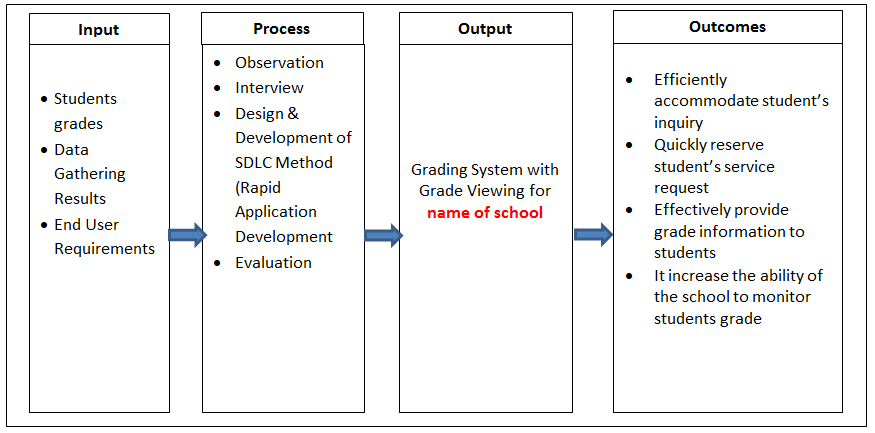
Healthcare consolidation in the form of mergers and acquisitions has been taking place for a number of years. It is seen on both the provider and payer sides. In his testimony on healthcare market’s consolidation effects on quality, cost and access, Paul Ginsberg, Director of Public Policy at the USC Schaeffer Center for Health Policy and Economics cites some key drivers of consolidation. ACOs require scaling which small hospitals cannot provide. Younger physicians prefer associations with larger enterprises. The costs for EHR and other technology acquisition and maintenance are too costly for smaller hospitals, and pressures of decreased payment rates are increasing on the provider side. Payers are consolidating as well because of pressures to scale for clients across large geographical regions and to support costs of technology. I would add that the enactment (and some would say the design) of the ACA itself spurred payer consolidation. It is interesting to note that a 2012 report by the Robert Wood Johnson Foundation on this topic concluded that hospital consolidation increases healthcare costs and that physician-hospital consolidation has neither improved quality of care or reduced costs. Healthcare consolidation on the other hand, might lead to internal cost savings with increased available resources to invest in technology. Certainly this remains to be seen. Consolidation includes both human and material resource consolidation. I will focus on areas where I believe technology can facilitate consolidation by addressing pain points.
Electronic health records purchase, maintenance, and associated technologies (analytics, digital imaging, patient monitoring, etc) are now necessary big-ticket items in healthcare. Unfortunately the timing of consolidation sometimes doesn’t coincide with optimal purchase evaluation and merging of technologies by the involved parties. This often results in the maintenance of multiple EHR vendors for inpatient systems and even more if one includes outpatient setting. There are large institutions in the USA who are decades past merging and still have disparate EHR systems which do not communicate with each other. Consolidation often results in providers needing to go to new hospitals or offices, necessitating training on new EHR systems. In addition, the current use of electronic portals by patients to view their medical record is abysmal. A survey by athenahealth reveals that although 87% of patients want electronic access to their medical records only 29% actually use portals. Both providers and patients usually have to negotiate diverse healthcare site-specific platforms. One potential solution lies in the adoption of a user-friendly universal EHR interface which provides a simple and standardized user experience on both provider and patient (portal) ends regardless of the EHR technology used.
Consolidation offers the opportunity for hospitals to reevaluate purchasing a new EHR system (as many already have or are considering). Healthcare IT can play a major role in M & A for providers. There are many considerations when EHRs collide.
Other non-clinical considerations. Some of the non-clinical areas include standardizing logistics and tracking. This relates to tracking of medications which can improve patient safety, tracking of patients which can increase effective bed capacity from 5-20%, and tracking of supply chain assets which connects inventory data with clinical/procedural data to streamline billing and avoid unexpected equipment shortages. Technologies which lend themselves to this include traditional bar coding, RFID (radio-frequency identification), and potentially blockchain, an advanced information technology well-established in the finance sector but presently only talked about in healthcare.
Clinical applications. Consolidation often brings together different institutional cultures. This may be reflected in how physicians, nurses and other clinical personnel are trained, compensated, and included in policy and procedural changes. Its extent includes but is not limited to clinical organizational structure, clinical policies, hospital drug/device formularies, referral networks, clinical research, medical education, and reassignment of workplaces. Patients are affected directly and indirectly. The immediate reaction of patients and caregivers is commonly apprehension. The patient’s clinical experience will be a significant priority in planning the logistics and final outcome of a consolidation plan. Marketers of the new entity will refocus on patient satisfaction. Brand loyalty might be a challenge in the case of purchasing or merging with a competitor. This presents opportunities for creating patient “stickiness.” The adoption of patient and caregiver-facing tools (which may include appointment apps, remote patient monitoring for self-management of chronic diseases, a standardized enhanced patient portal/communications platform, digital patient education tools, telehealth video conferencing, and others) can generate a message of patients as a priority. Instituting new system-wide clinician-facing tools including consolidated mobile digital imaging tools, communication tools, mobile inpatient telemetry apps, clinician scheduling/logistics/ communication tools, operating room video/patient monitoring, mobile clinical trial platforms, and best of breed medical and continuing education tools are ways to attract and retain top clinical talent.
Value based payment models. Consolidation in the era of value-based payment models presents opportunities for improvement of care. In fact arguments for consolidation are based on the promise of improved cheaper care. This has yet to be demonstrated (in healthcare or any other industry). This type of payment system shifts the ROI of digital technology from one based on revenue generation to cost savings. The significance of such a shift cannot be overstated because it ideally aligns cost with the presumed overriding objective of better patient outcomes. Remote patient monitoring, predictive analytics, and mobile technologies are being utilized by both providers directly and indirectly health management companies contracted by payers. The power of these tools resides in the data and analytics they hopefully deliver to providers, patients and caregivers in a filtered, actionable and easily digestible fashion.
In summary, consolidation in healthcare affords opportunities for technology to address pain points which are organizational, clinical, and image management in nature. The goal should not be for the imposition of the dominant partner of its operations but to seize the occasion to reshape the new entity to something even better via cohesive innovation.